Introduction
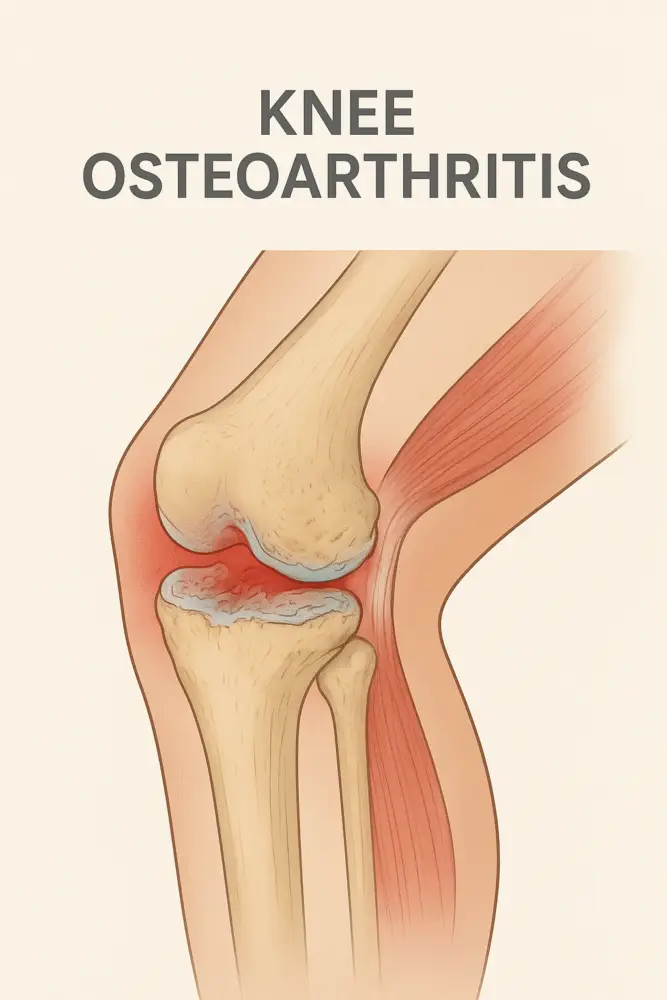
Knee osteoarthritis (OA) is a progressive degenerative joint condition characterized by the breakdown of articular cartilage, changes in the underlying bone, and inflammation of surrounding tissues. It is one of the leading causes of knee pain and disability in adults, particularly affecting individuals over the age of 50, although it can also occur in younger populations due to injury or mechanical stress.
Causes of Knee Osteoarthritis
The exact cause of knee osteoarthritis is often multifactorial, involving both mechanical and biological factors. Common causes include:
- Age-related degeneration – Natural wear and tear over time reduces cartilage elasticity and thickness.
- Previous knee injuries – Trauma, ligament injuries, or meniscal tears can accelerate joint degeneration.
- Genetic predisposition – A Family history of osteoarthritis can increase susceptibility.
- Excess body weight – Extra load on the knee joint increases stress and accelerates cartilage breakdown.
- Repetitive stress – Occupations or sports that involve frequent kneeling, squatting, or heavy lifting.
- Joint malalignment – Varus (bow-legged) or valgus (knock-kneed) deformities cause uneven cartilage wear.
- Metabolic disorders – Conditions such as diabetes or gout may contribute to joint deterioration.
Signs and Symptoms
Knee osteoarthritis develops gradually, with symptoms worsening over time. Common signs and symptoms include:
- Pain – Usually worsens with weight-bearing activities such as walking, climbing stairs, or standing for long periods.
- Stiffness – Especially after periods of inactivity or in the morning (morning stiffness typically lasts less than 30 minutes).
- Swelling – Due to inflammation and excess synovial fluid.
- Crepitus – Grinding, crackling, or popping sensation during joint movement.
- Reduced range of motion – Difficulty in bending or straightening the knee.
- Joint deformity – Advanced stages may show visible changes in knee alignment.
Diagnostic Physical Tests
A clinical examination combined with imaging confirms the diagnosis of knee OA. Common physical tests include:
- Observation and Palpation
- Inspect for swelling, deformity, muscle wasting, and abnormal gait patterns.
- Palpate for joint line tenderness, bony enlargements, or warmth.
- Range of Motion (ROM) Testing
- Assess both active and passive knee flexion and extension.
- Compare with the unaffected side.
- Crepitus Test
- Gentle movement of the patella or knee joint to feel for grinding sensations.
- Gait Analysis
- Identifies limping, reduced stride length, or compensatory movements.
- Patellofemoral Compression Test
- Applying pressure on the patella while the patient contracts the quadriceps, pain indicates patellofemoral joint involvement.
- Imaging Studies
- X-ray: Reveals joint space narrowing, osteophyte formation, and subchondral sclerosis.
- MRI: Detects early cartilage damage and associated soft tissue injuries.
Rehabilitation Protocol for Knee Osteoarthritis
The goal of rehabilitation is to relieve pain, enhance mobility, build supporting muscle strength, and slow the disease’s advancement. A comprehensive physiotherapy protocol includes:
1. Patient Education
- Understanding OA and its management helps patients stay motivated.
- Guidance on joint protection techniques, activity modification, and pacing strategies.
2. Pain Management
- Modalities: Hot packs, cold therapy, ultrasound, or TENS for pain relief.
- Medications: NSAIDs or topical analgesics (under physician guidance).
Key Exercises for Knee Osteoarthritis
Heel Slides
Isometric quad contractions
Isometric quad contractions
Straight leg raises
Hamstring Strengthening
Hamstring Strengthening
Side-lying leg raises
Clamshells
5. Balance and Proprioception Training
- Standing on one leg
- Mini-squats on a stable or unstable surface
6. Aerobic Conditioning
Low-impact activities such as walking, cycling, or swimming.
Functional Training
- Sit-to-stand practice
- Step-ups and controlled stair climbing
8. Assistive Devices
Use of canes, knee braces, or orthotics to offload pressure from the affected joint.
Prevention and Long-Term Care
- Maintain a normal body weight to reduce knee stress.
- Stay physically active to keep muscles strong.
- Avoid high-impact sports or activities that overload the knees.
- Wear proper footwear for shock absorption and stability.
Conclusion
Knee osteoarthritis is a chronic condition that requires early detection and comprehensive management to slow its progression. A combination of lifestyle modifications, physiotherapy, and medical interventions can help patients maintain mobility, reduce pain, and improve quality of life. Rehabilitation plays a crucial role in preserving function and enabling individuals to remain active despite the degenerative nature of the disease.




Genuine and excellent way of describing osteoarthritis, its diagnosis, causes, symptoms, and also key exercises necessary for treatment of osteoarthritis.
As someone who’s played every car game under the sun, Blocky Car’s minimalist approach is refreshing. The handling model reminds me of early arcade racers, and the custom parts system has serious depth. Definitely worth grinding for those rare upgrades!